Introduction
Executive Summary
B-Secur is revolutionising cardiac health monitoring with its proprietary HeartKey® technology, addressing the critical issue of noise in ECG data that impacts remote monitoring systems.
Our FDA 510(k) cleared HeartKey software processes ECGs with clinical-grade accuracy, enhancing interpretation and improving clinical workflows. HeartKey has been shown to reduce low-quality events requiring review by 40.6% and our filtering techniques have been shown to reduce the amount of data deemed undiagnosable due to noise by 9.7% and improve rhythm classification accuracy by 4.9%. This white paper details our innovative approach, robust R&D efforts, and the transformative impact of HeartKey® on healthcare systems.
Who Is B-Secur?
B-Secur are at the forefront of the next generation of wellness and healthcare solutions, blending our expertise in engineering with the demands of modern medical technology. We are committed to enhance the quality of data from wearables and medical devices, from smartwatches to patches, improving efficiency and accuracy. Our Professional Services team works directly with engineers, empowering them to make optimised design decisions, while our proprietary ECG algorithms enhance the signal and create clarity for our healthcare staff.
Our Mission
Our mission is to advance biosensing technology that enables a new level of care and creates growth opportunities for our partners in the health and wellness markets.
Our Motivation: A Response to a Growing Need
B-Secur is driven by a critical observation: the rising prevalence of cardiovascular diseases (CVD) worldwide, accounting for 20 million deaths annually1, up to 90% of which are preventable2. Traditional cardiac monitoring methods face significant challenges, including pervasive issues with signal noise, particularly in ambulatory settings. This noise can obscure critical data, leading to delays in care, misdiagnoses, and inefficient resource use. Our flagship technology, HeartKey, is designed to directly address these challenges, offering a robust solution that enhances data clarity and accuracy, ultimately improving patient outcomes.
Innovative Approach to Cardiac Monitoring
HeartKey is not just a solution; it’s a revolution in cardiac health monitoring. With over eight years of dedicated research and development, our team initially began by exploring the use of ECG signals for biometric authentication. Focusing on the unique requirements of this technology, including dry electrode utilisation and high accuracy ECG acquisition, lead us to tackling noise reduction head-on. By leveraging expertise from fields such as automotive and semiconductor technologies, we’ve significantly enhanced the fidelity and utility of traditionally challenging ECGs, unlocking their potential for cardiac health monitoring.
Teamwork at the Core
Our diverse R&D teams are the backbone of B-Secur. Each team brings specialized expertise, from enhancing the fidelity of biosignals to integrating these advancements seamlessly into consumer and medical devices. This collaborative effort ensures that our products are not only cutting edge but also practical and user-centric.
Understanding ECG Noise: Sources, Implications, and Prevalence
Sources of Noise in ECG Monitoring
ECG recordings are critical for diagnosing and monitoring cardiac health but are susceptible to various types of noise that can significantly degrade data quality. These sources of noise fall into two primary categories: corporeal and technical.
Corporeal Sources: These are physiological in origin and include baseline wander — typically caused by respiration or patient movement — muscle noise, which arises from electromyographic signals due to muscle contractions, and electrode noise, originating from movement at the electrode-skin interface.
Technical Sources: These encompass a range of artificial interferences such as powerline interference, which results from the electrical supply, and noise introduced by other medical equipment.
Implications and Prevalence of ECG Noise Interference
ECG noise interference has serious clinical implications. Artifacts resembling arrhythmias can mislead clinicians and automated systems, resulting in inappropriate therapeutic interventions and unnecessary diagnostic procedures, which increase patient distress and healthcare costs3. Additionally, severe noise interference can render significant portions of ECG recordings clinically unactionable, creating additional clinical burdens and inefficiencies4. This often necessitates repeat investigations to obtain usable data, delaying therapeutic treatment and potentially leading to poorer patient outcomes.
The prevalence of noise in cardiac monitoring is a well-recognized issue within the medical community. Studies indicate that over 53% of remote ECG monitoring systems are affected by noise, impacting their clarity and utility5. 92% of healthcare professionals have reported significant noise contamination necessitating repeat investigations in ≥10% of ECGs acquired during clinical practice6.
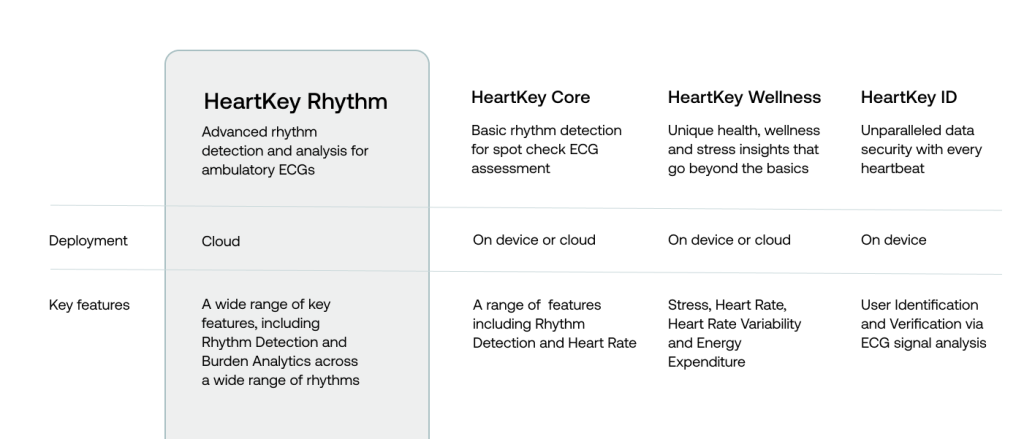
Introducing HeartKey Rhythm: A Leap in Cardiac Health Technology
The Development Journey of HeartKey Rhythm
Following rigorous research and development, B-Secur launched HeartKey at CES (Consumer Electronics Show) 2019, and shortly after, received FDA 510(k) clearance for the HeartKey health algorithms in early 2020. B-Secur is now proud to introduce HeartKey Rhythm, an FDA 510(k) cleared, groundbreaking advancement in the field of ECG processing and analysis software. HeartKey Rhythm embodies our commitment to innovation, built on a foundation of over 2 million hours of consumer and medical ECG data, translating to more than 8 billion heartbeats analysed. This extensive data has allowed us to refine our algorithms to provide unmatched accuracy and reliability in ECG processing and analysis.
Regulatory Approval and Quality Assurance
FDA 510(k) clearance of HeartKey Rhythm (K233755), affirms that it not only meets but exceeds the stringent safety and efficacy requirements of medical device software. This clearance is a testament to the quality-focused approach that has been a cornerstone of our development process from the start.
Advisory and Supportive Role in Clinical Settings
HeartKey Rhythm is designed to complement and enhance the clinician’s expertise, not replace it. By delivering high-quality ECG processing and analysis, HeartKey Rhythm supports clinicians in making informed decisions. It provides reliable data that clinicians can use to better understand ECG patterns, patient history, and other diagnostic information, allowing their expertise to truly shine and ensure optimal patient care.
Designed for Facile Integration and Versatility
HeartKey Rhythm is a cloud-based software library specifically designed to process ECGs in challenging ambulatory environments. It seamlessly integrates within the signal processing chains of various medical devices, including Holter monitors, ECG patches, and Mobile Cardiac Telemetry (MCT) systems. A key advantage of our technology is its deployment as a Docker container; a flexible, standalone package that includes everything needed to run the software, ensuring that no patient data ever leaves your system, offering complete control over data security and privacy.
Features and Clinical Benefits
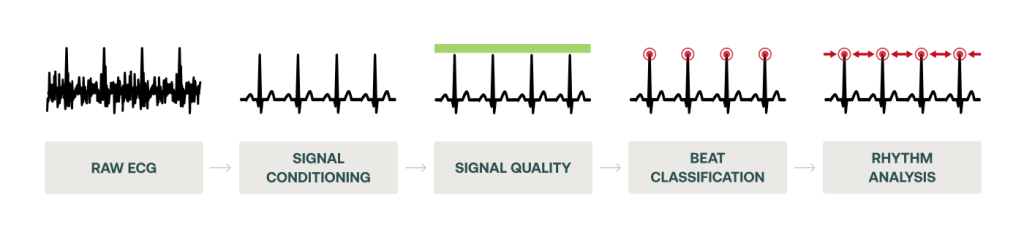
HeartKey Rhythm provides a suite of advanced ECG signal processing and analysis algorithms designed to streamline ECG workflow and aid clinical decision-making.
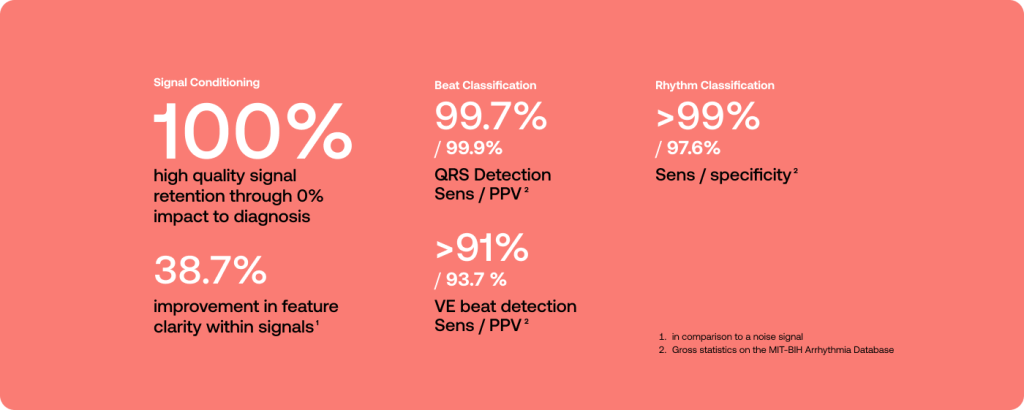
- Signal Conditioning: HeartKey Rhythm employs adaptive filtering techniques to target and remove common sources of ECG noise interference, such as baseline wander, muscle noise, and powerline interference, and enhance signal clarity. This preprocessing step is crucial for maintaining the fidelity of the ECG signal, particularly in ambulatory settings where movement and external electrical noise can distort readings.
- Signal Quality Assessment: Before any critical analyses occur, HeartKey Rhythm evaluates the signal quality to identify and flag low-quality signals, allowing only high-quality ECGs to proceed to triage for arrhythmia assessment. By ensuring that only high-quality data is analysed, we minimize the risk of diagnostic errors associated with noise, both by healthcare professionals and downstream interpretation algorithms. Additionally, this allows healthcare professionals to focus on meaningful, actionable data, without the distraction of unactionable data, therefore improving efficiency in the clinical workflow.
- Beat Analysis: Accurate beat detection is fundamental to all subsequent ECG analysis. HeartKey Rhythm excels in this area, with robust algorithms that ensure precise detection and classification of normal beats and ventricular ectopic (VE) beats. By mastering this essential aspect, we provide a reliable foundation for all downstream algorithms, ensuring the highest accuracy and confidence in our ECG analysis.
- Heart Rate Detection: HeartKey Rhythm includes advanced heart rate detection algorithms designed to provide precise and reliable heart rate measurements.
- Rhythm Analysis: The rhythm analysis feature leverages the cleaned signals, along with their accurately identified beat types and locations, to perform a comprehensive evaluation that can detect the most common cardiac rhythms. This analysis aids clinicians in diagnosing a range of cardiac abnormalities, providing a deeper insight into the patient’s cardiac health.
HeartKey Rhythm Validation
Comprehensive validation ensures reliability in diverse monitoring scenarios, which is why this was an absolute priority during the development of HeartKey Rhythm. Each aspect of HeartKey Rhythm was independently validated to ensure optimal performance.
Case Study 1: Enhancing the Efficiency and Accuracy of ECG Interpretation Through Digital Denoising with HeartKey
Background
The interpretation of ECGs is a crucial skill in healthcare, used across various medical disciplines to diagnose and manage cardiac issues. Adept interpreters rely on a combination of pattern recognition capabilities and advanced cognitive functions to discern pathological deviations in the ECG, contingent upon the clear identification of diagnostic features. However, deficiencies in the ECG interpretation abilities of healthcare professionals are a longstanding concern within the medical community. Major errors have been reported in up to 33% of ECG interpretations7, and as many as 11% of these errors lead to inappropriate patient management8. Recent studies have highlighted the considerable variation in ECG interpretation accuracy between healthcare professions and experience levels9,10.
Among training and educational factors that impact the ability of healthcare professionals to interpret an ECG accurately and confidently, the presence of noise and artefacts originating from non-cardiac sources can play a significant role. Artefacts that mimic the morphology of pathological features can simulate non-existent arrhythmias and cardiac abnormalities, including atrial fibrillation, ventricular tachycardia, and myocardial ischemia, resulting in erroneous diagnoses and potentially inappropriate interventions. Furthermore, excessive noise interference can distort or obscure the underlying signal, rendering significant portions of recordings clinically unactionable. This can potentially result in missed or delayed diagnoses, a problem that is exacerbated in the ambulatory setting.
The Challenge
Despite the established correlation between noise and erroneous diagnoses, research evaluating the impacts of digital denoising software on clinical ECG interpretation ability of healthcare professionals is lacking, making it difficult to justify the integration of innovative technologies like HeartKey within clinical workflows.
Study Aims
B-Secur, in collaboration with the Allan Lab at Jersey General Hospital, conducted this pivotal study to explore the impact of advanced digital denoising software (HeartKey) on improving the interpretive capabilities of healthcare professionals (lacking in the literature).
Study Design
The study involved a diverse cohort of 48 healthcare professionals with a range of different experience levels, who assessed a series of single-lead ECG recordings using a blinded protocol that compared their ability to confidently diagnose cardiac rhythms with and without the aid of HeartKey denoising.
Impacts on Interpretive Capabilities
Signal denoising through HeartKey significantly improved diagnostic rhythm classification accuracy and confidence among the healthcare professionals (relative to raw signals):
- 4.9% increase in rhythm classification accuracy.
- 6.2% improvement in diagnostic confidence.
- 9.7% reduction in data deemed undiagnosable.
Participant comments on the impact of HeartKey on the interpretive process:
“More confidence in my diagnosis with less ECG artifact” – Participant 16, Cardiologist
“Improves confidence, as the raw strip has significant area of interference and therefore difficult/unable to use” – Participant 14, Junior Doctor
“Significant removal of baseline artefact revealing AF more easily” – Participant 5, Consultant Cardiologist
Participant Perception of HeartKey Denoising
Participants had a predominantly positive perception of digital denoising as it relates to the three aspects of clinical ECG workflow that were assessed:
- 51% stated a ‘positive’ or ‘very positive’ impact of HeartKey on revealing previously unseen pathologies in the raw signal.
- 65% stated a ‘positive’ or ‘very positive’ impact of HeartKey on speeding up diagnosis
- 74% stated a ‘positive’ or ‘very positive’ impact of HeartKey on improving the ease of ECG readability
Implications for Clinical Workflow
The findings from this study underline the potential of digital denoising technology to transform ECG interpretation practices. By integrating HeartKey into their workflow, healthcare providers can achieve:
- Quicker, more confident decision-making based on clearer ECG data.
- Fewer diagnostic errors due to noise, leading to better patient outcomes.
- Reduced healthcare costs and improved efficiency by minimizing the need for repeated tests.
Conclusions
This case study highlights B-Secur’s commitment to pioneering solutions that address practical challenges in cardiac care. HeartKey’s ability to enhance the interpretive accuracy and confidence of ECG data not only supports healthcare professionals in their daily duties but also aligns with broader goals of improving patient care through technological innovation.
Case Study 2: Reducing the Review Burden of Unactionable Ambulatory ECG Signals
Background
Ambulatory ECGs are fundamental tools in the diagnosis and monitoring of cardiac conditions, providing critical insights into cardiac function over extended periods. Traditionally, these ECGs are used in settings where continuous monitoring is necessary to capture transient or infrequent cardiac events that might not be detected during a standard 12-lead ECG. The presence of noise and artefacts in ECG recordings complicates the diagnostic process, requiring healthcare professionals to spend considerable time distinguishing between poor-quality, non-actionable data and clinically relevant signals. This differentiation is critical because erroneous interpretations due to noise can lead to misdiagnoses or unnecessary further testing, both of which have implications for patient safety and healthcare costs.
The Challenge
The high prevalence of noise in ambulatory ECGs poses a substantial challenge, with healthcare professionals often needing to manually review large volumes of ECG data, a process that is both time-consuming and prone to human error. Although signal quality assessment algorithms have been hailed as solutions to reduce the review burden of unactionable ECG, the integration of such features within standard clinical practice has been slow, primarily due to a lack of evidence-based research highlighting the potential benefits they can endow.
Study Aims
The primary aim of this study was to evaluate the impact of HeartKey Rhythm’s Signal Quality algorithm on the clinical workflow of an Independent Diagnostic Testing Facility (IDTF). By integrating automated signal quality indicators, we sought to reduce the time healthcare professionals spend reviewing unactionable ECG data, thereby enhancing workflow efficiency.
Study Design
We conducted a two-phase study on patients who were referred to an IDTF (TZ Medical, Tualatin) for continuous cardiac monitoring, utilizing a three-channel cardiac monitor (Trident®). The HeartKey Signal Quality algorithm was employed to evaluate each ECG lead, segmenting the data into two-second intervals classified as either high or low quality. The overall event quality was determined based on the proportion of low quality segments, with validations against manual annotations. As signal quality is not often consistent across all recorded leads, we employed an aggregate metric derived from the highest quality lead per event to represent the best-case scenario.
Phase 1
A retrospective analysis of 19,392 ECG arrhythmia events from 291 patients. This phase focused on defining an optimal threshold of low quality data to be automatically discarded prior to ECG triage, while also maintaining minimal risk of discarding actional data. At a threshold where >90% of an event had been classified by HeartKey as low quality, the IDTF were able to reduce the number of unactionable events that required manual review by 32.4%, with only a negligible 0.3% chance of discarding actionable data.
Phase 2
A prospective, two-arm analysis of 33,249 events over a one-week period. Events ranged from 60-180-seconds (mean: 72 seconds) and totalled 669 hours of ECG data. This phase involved further optimisation of the thresholds identified in Phase 1, which resulted in a change of focus from percentage of unactionable data to duration of unactionable data. Healthcare professionals determined that <8-seconds of combined high quality data across the aggregate lead would be deemed unactionable, translating to a proportional threshold, as defined in Phase 1, ranging from 87.7% to 95.6%. Utilising this new threshold of <8-seconds of high quality data enabled a reduction in all ECG events requiring manual review by 17.1%, with a reduction in artefact events by a staggering 40.6%, while still maintaining a specificity of 99.8%.

An overview of the study design (*results compared to outputs from ECG Tech Review during live triage of events)
Implications for Clinical Workflow
The integration of HeartKey Signal Quality indicators into the ECG review process ensured that healthcare professionals spent their time reviewing only the most clinically relevant data by significantly reducing the volume of data requiring manual review. For a healthcare professional reviewing 50 events per day at an average two-minute review time per event, this equates to a daily time saving of >17 minutes, enabling the review of an additional 8.6 events per day.
Conclusions
The implementation of automated signal quality indicators within the ECG review workflow presents a substantial advancement in the management of ambulatory ECG data. By significantly reducing the time clinicians spend on reviewing unactionable data, HeartKey enables more efficient patient monitoring and potentially quicker diagnostic turnaround. This case study underscores B-Secur’s commitment to enhancing the utility and efficiency of cardiac monitoring technologies in clinical settings.
Case Study 3: A Case of Persistent False Atrial Fibrillation Detection by a Smartwatch Algorithm
Background
Apprehensions regarding the accuracy of atrial fibrillation (AF) detection by smartwatch algorithms persist despite their growing popularity. As false positive AF alerts can negatively impact a patient’s perceived physical wellbeing and confidence in managing chronic symptoms, understanding the potential sources of algorithmic error is crucial for informed patient care.
The Challenge
Smartwatch ECGs are acquired in uncontrolled environments, subjecting these signals to less-than ideal recording conditions. This, paired with the unique ECG morphology across a real-world population, increases the likelihood for false results, which when received by a lay person, may raise stress levels and health anxiety.
Study Aims
The primary aim of this study was to identify limitations in smartwatch acquired ECGs including their generalisability across a real-world population, highlighting the importance of independent validation through the HeartKey Rhythm Classification algorithm when assessing the reliability of consumer ECG data.
Study Design
A 38-year-old male with intermittent palpitations, clamminess, and lightheadedness developed anxiety after receiving multiple ‘Atrial Fibrillation’ (AF) alerts from his smartwatch ECG (Samsung® Galaxy Series 4). Prompted by an ‘unusual sensation in the heart’, a familial history of MI, and a perceived worsening of symptoms, the patient presented at the Emergency Department, where a 12-lead ECG revealed a normal sinus rhythm of 90 bpm. The patient was reassured, discharged in a calm state, and referred for cardiological consultation. Holter monitoring on three subsequent occasions, echocardiographic examination, and coronary CT all proved unremarkable. Despite this, the patient continued to receive false AF triggers, resulting in ongoing anxiety and health issues. A troubleshooting session confirmed proper device use and revealed that all AF alerts were false, with the patient actually in sinus rhythm. Notably, the erroneous interpretations did not align with common sources of algorithmic error, such as artefact or ectopy, and manifested in signals of both high and low quality. A consistent feature was the patient’s atypical waveform which deviated from a typical smartwatch signal resembling Einthoven Lead I. To provide reassurance, the false positive data was extracted and re-analysed using HeartKey®, which correctly identified signals as either sinus rhythm or inconclusive.
Conclusion
This case study raises questions around the universality of AF detection on consumer devices such as smartwatches and underscores the need for improved clarity and accountability in the design and deployment of such technologies. The importance of independent validation of consumer ECG data is highlighted through results returned by HeartKey.
Conclusion
B-Secur’s HeartKey technology emerges as a pivotal innovation in cardiac health monitoring. Our advanced filtering techniques and robust signal processing significantly reduce noise in ECG data, leading to better diagnostic accuracy and streamlined clinical workflows. We remain committed to pushing the boundaries of innovation and ensuring quality in every aspect.
Why Choose HeartKey Rhythm?
- Proven Performance: Validated on over 8 billion beats to ensure performance in a variety of challenging environments
- Regulatory Assurance: With FDA 510(k) clearance, HeartKey meets high standards for safety and efficacy.
- Versatile Deployment: HeartKey offers flexible deployment as a Docker container, fitting seamlessly into various clinical environments and ensuring that no patient data ever leaves your system, offering complete control over data security and privacy.
Call to Action
Embrace the next generation of cardiac health monitoring, offering superior clarity, accuracy, and efficiency. We urge healthcare providers, medical device manufacturers, and technology partners to collaborate with us in this transformative endeavour. By integrating HeartKey into your systems, you can elevate patient care, streamline workflows, and combat the global challenge of cardiovascular diseases.
Citations
1 https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
2American Heart Association – CDC Prevention Programs | American Heart Association. Retrieved April 25, 2022, from www.heart.org/en/get-involved/advocate/federal-priorities/cdc-prevention-programs
3 El-Sherif, N. & Turitto, G. Ambulatory electrocardiographic monitoring between artifacts and misinterpretation, management errors of commission and errors of omission. Ann. Noninvasive Electrocardiol. 20, 282-289 (2015).
4 Karaoğuz, M. R. et al. The quality of ECG data acquisition, and diagnostic performance of a novel adhesive patch for ambulatory cardiac rhythm monitoring in arrhythmia detection. J. Electrocardiol. 54, 28-35 (2019).
5 Survey of >1,600 EPS; Ding EY. Cardiovasc DigitHealth J. 2020.
6 McKenna S, et al. Evaluating the impacts of digital ECG denoising on the interpretive capabilities of healthcare professionals, Eur Heart J Dig Health. 2024; ztae063.
7 Mele P. Improving electrocardiogram interpretation in the clinical setting. J Electrocardiol 2008;41:438-439.
8Breen CJ, Kelly GP, Kernohan WG. ECG interpretation skill acquisition: A review of learning, teaching and assessment. J Electrocardiol 2022;73:125-128.
9Cook DA, et al. Accuracy of physicians’ electrocardiogram interpretations: a systematic review and meta-analysis. JAMA Intern Med 2020;180:1461–1471.
10Kashou AH, et al. ECG interpretation proficiency of healthcare professionals. Curr Probl Cardiol 2023;48:101924.